The Cause And Treatment Of Posterior Tibial Tendon Dysfunction
Overview
Adult acquired is a very serious condition that can lead to many secondary deformities, not only within the foot but also in the knees, hips and back. This presentation discusses a new scientifically proven procedure that may be able to help realign and fix this problem at its root. 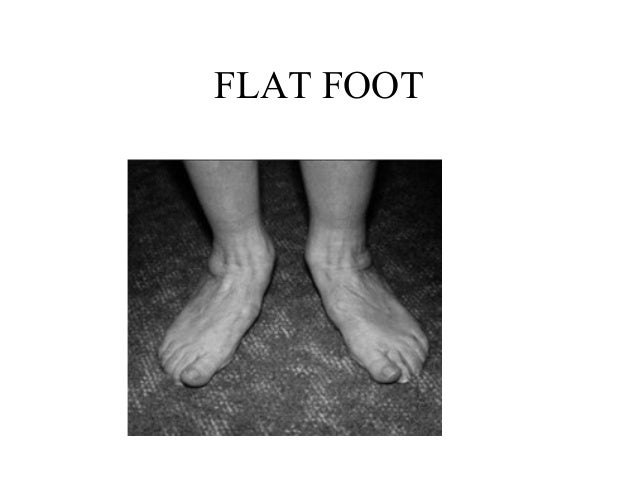
Causes
Many health conditions can create a painful flatfoot, an injury to the ligaments in the foot can cause the joints to fall out of alignment. The ligaments support the bones and prevent them from moving. If the ligaments are torn, the foot will become flat and painful. This more commonly occurs in the middle of the foot (Lisfranc injury), but can also occur in the back of the foot. In addition to ligament injuries, fractures and dislocations of the bones in the midfoot can also lead to a flatfoot deformity.
Symptoms
Symptoms shift around a bit, depending on what stage of PTTD you?re in. For instance, you?re likely to start off with tendonitis, or inflammation of the posterior tibial tendon. This will make the area around the inside of your ankle and possibly into your arch swollen, reddened, warm to the touch, and painful. Inflammation may actually last throughout the stages of PTTD. The ankle will also begin to roll towards the inside of the foot (pronate), your heel may tilt, and you may experience some pain in your leg (e.g. shin splints). As the condition progresses, the toes and foot begin to turn outward, so that when you look at your foot from the back (or have a friend look for you, because-hey-that can be kind of a difficult maneuver to pull off) more toes than usual will be visible on the outside (i.e. the side with the pinky toe). At this stage, the foot?s still going to be flexible, although it will likely have flattened somewhat due to the lack of support from the posterior tibial tendon. You may also find it difficult to stand on your toes. Finally, you may reach a stage in which your feet are inflexibly flat. At this point, you may experience pain below your ankle on the outside of your foot, and you might even develop arthritis in the ankle.
Diagnosis
The diagnosis of tibialis posterior dysfunction is essentially clinical. However, plain radiographs of the foot and ankle are useful for assessing the degree of deformity and to confirm the presence or absence of degenerative changes in the subtalar and ankle articulations. The radiographs are also useful to exclude other causes of an acquired flatfoot deformity. The most useful radiographs are bilateral anteroposterior and lateral radiographs of the foot and a mortise (true anteroposterior) view of the ankle. All radiographs should be done with the patient standing. In most cases we see no role for magnetic resonance imaging or ultrasonography, as the diagnosis can be made clinically.
Non surgical Treatment
Options range from shoe inserts, orthotics, bracing and physical therapy for elderly and/or inactive patients to reconstructive surgical procedures in those wishing to remain more active. These treatments restore proper function and alignment of the foot by replacing the damaged muscle tendon unit with an undamaged, available and expendable one, lengthening the contracted Achilles tendon and realigning the Os Calcis, or heel bone, while preserving the joints of the hindfoot. If this condition is not recognized before it reaches advanced stages, a fusion of the hindfoot or even the ankle is necessary. Typically this is necessary in elderly individuals with advanced cases that cannot be improved with bracing. 
Surgical Treatment
Many operations are available for the treatment of dysfunction of the posterior tibial tendon after a thorough program of non-operative treatment has failed. The type of operation that is selected is determined by the age, weight, and level of activity of the patient as well as the extent of the deformity. The clinical stages outlined previously are a useful guide to operative care (Table I). In general, the clinician should perform the least invasive procedure that will decrease pain and improve function. One should consider the effects of each procedure, particularly those of arthrodesis, on the function of the rest of the foot and ankle.